Dr. Mark Blumenkranz Previews Panel on OCT Imaging and Forum on Laser-Based Imaging
Regulatory and reimbursement issues surrounding laser-based imaging modalities such as optical coherence tomography and adaptive optics, as well as the emerging role of artificial intelligence in ophthalmic imaging, will be the focus of a multi-disciplinary workshop with a host of medical organizations and the Food and Drug Administration April 8 in Silver Spring, MD, a suburb of Washington, DC.
The Forum on Laser-Based Imaging planning committee involved participants from the American Academy of Ophthalmology, American Glaucoma Society, American Society of Cataract and Refractive Surgeons, and American Society of Retinal Specialists, among others. Among the FDA officials expected to be in attendance is Malvina Eydelman, MD, director of the Division of Ophthalmic, and Ear, Nose and Throat Devices at the FDA’s Center for Devices and Radiological Health.
Optical Coherence Tomography Panel
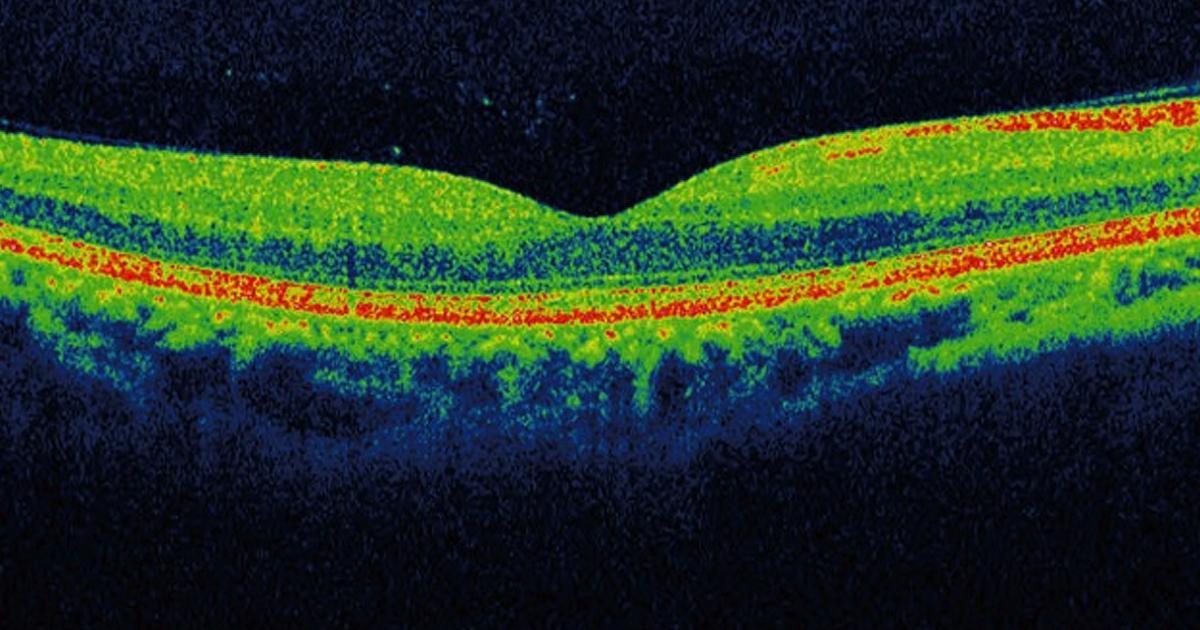
Mark S. Blumenkranz, MD, H.J. Smead Professor emeritus and director of the Ophthalmology Innovation Program at Stanford University’s Byers Eye Institute, will moderate a discussion on innovation in OCT as part of the overall OCT session. The panel conversation will center around technology advancements and key aspects of the regulatory process that researchers and clinicians should consider when developing new products. Further, presenters are expected to explain how they are using artificial intelligence (AI) for automated and enhanced interpretation of data.
“We will have some outstanding people, talking about things in development now and excellent developments on the horizon,” Dr. Blumenkranz tells OIS Weekly. “We’ll also talk about the role that the FDA, academia, and companies play in facilitating innovation and how they all can work together to create new technology and get it approved and out to the clinic to benefit patient care.”
Addressing the use of AI to enable physicians to evaluate OCT images and data to refine predictive factors of disease progression will be Michael D. Abramoff, MD, PhD, founder and CEO of IDx Technologies; Theodore Leng, MD, MS, a retina specialist at Byers Eye Institute; and Nadia Waheed, MD, MPH, associate professor of ophthalmology at Tufts University School of Medicine.
Role of AI in Diagnostics
Dr. Abramoff’s company was the first to receive FDA approval for an AI device to detect diabetic retinopathy. The device’s algorithm has been shown to accurately make a diagnosis for this disease based on a fundus camera’s images of a patient’s retina, and Dr. Blumenkranz envisions a time that similar and enhanced capabilities will exist for images from other systems, such as OCT.
Dr. Leng, an expert in macular disease, is developing AI technology to interpret OCT scans to not only analyze a patient’s current eye health, but also to predict whether the eye is at risk for more serious progressive disease in the future. Dr. Waheed, a national authority on OCT use for detecting retinal disease, is expected to talk about her work developing new algorithms to detect subtle changes in the retina.
“We will be discussing the use of AI and we will look at whether you can rely on AI to evaluate the retina and make the subtle judgments that only humans have been able to make, until now,” Dr. Blumenkranz says.
Glaucoma and Other Applications
Glaucoma specialists Lama Al-Aswad, MD, MPH, associate professor of ophthalmology at Columbia University Medical Center, and Felipe Medeiros, MD, professor of ophthalmology at Duke University School of Medicine, are expected to explore new uses of OCT to detect and treat glaucoma. Dr. Medeiros has been studying the use of OCT to examine the shape of the front of the eye, as well as to analyze optic nerve cell layers to try to catch and treat the disease earlier.
Mays El-Dairi, MD, a pediatric neuro-ophthalmologist at the Duke Center for Autism and Brain Development, is to present her work on developing techniques to identify optic nerve disease in children. Often, pediatric optic nerve disease goes undetected until it is too late to save the child’s vision.
Alastair Denniston, MA, MRCP, PhD, consultant ophthalmologist and honorary professor at the University of Birmingham’s Institute of Inflammation and Ageing, is expected to talk about his work on developing OCT clinical research standards to effectively enable the development of drugs for treating inflammatory eye disease.
Frank Brodie, MD, a postdoctoral innovation fellow in ophthalmology at Stanford Medicine, plans to talk about the regulatory process.
Brad Cunningham, MSE, RAC, an FDA branch chief, supervisory biomedical engineer, and acting associate director of the Office of Health Technology at the U.S. Public Health Services’ Center for Devices and Radiological Health, will explain how medical device studies need to be structured, which data endpoints should be used, and the process of regulatory approval.
“We’ll be looking for people to come away with a fuller and richer understanding of all the considerations that go into developing technology for specific-use cases,” Dr. Blumenkranz says. “To think about the regulatory approach early on, in terms of what the FDA wants to see before a device gets a premarket assessment and the best ways to choose endpoints and trial design to prove what you are doing is both safe and effective.”
Besides the session on OCT, later sessions will explore adaptive optics, nonclinical data sources, and reimbursement.
For questions about this article, contact bara.vaida@gmail.com.
